Abstract
Background: Red blood cell transfusion dependence (RBC-TD) is a reality for most MDS patients at some point during their disease trajectory. RBC-TD has been associated with inferior quality of life, iron overload and inferior overall survival. Alongside a focus on new therapies to abrogate or diminish the dependence on RBC units, optimizing quality of life while on transfusions may also have value. Our objective was to better understand the transfusion experience and what patients value, in order to inform future research initiatives. Methods: We designed a web-based survey (using SurveyMonkey) in the USA, Canada and UK that was disseminated by the international MDS Foundation, the Leukemia Lymphoma Society of Canada, the Aplastic Anemia and MDS Association of Canada (AAMAC), the University of York, the MDS registry of Canada and the MDS UK Patient Support Group. The survey consisted of 57 questions and was completed by willing patients who received at least 1 unit of blood in the previous 8 weeks. The anonymized survey was completed from 8/27/17 to 2/18/2018.
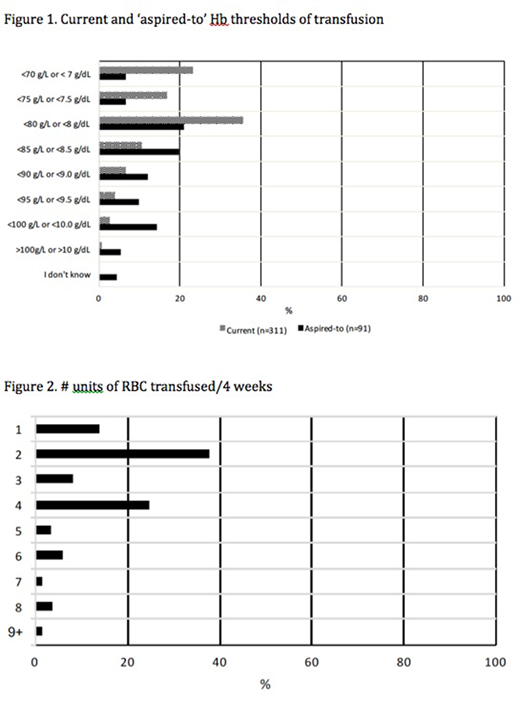
Results: Of 712 responses, 475 (67%) were RBC-TD and eligible for the survey. 55% were male with a median age of 72 years, 77% lived in urban or suburban communities. 75%, 12% and 12% of respondents were from USA, Canada and the UK; 93% were Caucasian. 45% and 27% reported lower and higher risk MDS respectively while 28% did not know. Patients reported having lived with MDS for a median of 3 years, 52% became transfusion dependent within 6 months of diagnosis and 37% > 12 months after diagnosis. 80% knew the haemoglobin (Hb) threshold at which they were transfused (Figure 1). 14%, 30% and 54% received 1, 1-2 or 2 units at a time and the median number of units/month was 2 (Figure 2). The most common symptoms pre-transfusion were fatigue (91%), weakness (69%), shortness of breath (SOB, 72%), dizziness (43%) and headache (22%) with fatigue and SOB having the most negative impact on their lives. 25%, 53% and 12% felt better after a transfusion within 1 day, 1-2 days and 3-4 days respectively and 20% felt worse for 1-2 days post transfusion. 64% reported feeling symptomatic for 5+ days before their next transfusion was organized, but 65% were able to organize a blood transfusion within 1-2 days of reaching their Hb threshold. 61% had a crossmatch on a different day from their transfusion and 30% of these patients indicated that they would have preferred to have a same day crossmatch even if it demanded more time at the transfusion centre. 42% were driven to their transfusions by friends or family. Travel time to the transfusion centre was < 1 hour for 93% of patients and did not have a negative impact on quality of life for 81% of respondents. 47% spent 4-6 hours at the clinic on the day of their transfusions and 19% spent 6-7+ hours. 31% faced economic hardship ('significantly' 12%, 'somewhat' 20%) due to their transfusion dependence. 24% experienced negative side effects consisting of, allergic reactions (32%), fever (16%), circulatory overload (9%), and other (39%). 57% patients reported iron overload. When presented with scenarios, 45% indicated that receiving less frequent transfusions (for example, by receiving 3 units at a time instead of 2) and 74% indicated that having home Hb point of care testing (to facilitate organizing transfusions before symptoms) would improve their QOL. Only 20% felt that receiving more frequent transfusions would improve their QOL, but 40% preferred to be transfused at a higher threshold than currently ordered by their physician. The ideal 'aspired-to' Hb thresholds for transfusion by these patients are indicated in figure 1, and 66% indicated a Hb of > 85g/L. Conclusions: It is well known that transfusion dependence has a negative impact on the QOL of MDS patients but this survey revealed that it also presents an economic hardship and significant time commitment. Patient feedback from this survey suggests some approaches that might improve the experience of TD MDS patients. These might include strategies to reduce the time for the transfusion pathway (eg. same day crossmatches) and point of care testing for Hb at home. Studies are needed to address a lack of evidence on optimal or higher Hb thresholds for red cell transfusion in outpatients as no trials have been conducted. 2 clinical trials (RBC-Enhance, NCT 02099669 and REDDS, ISRCTN26088319) are ongoing. More transfusion clinical trials with primary endpoints of patient reported outcomes are needed in MDS.
Buckstein:Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal